In 2007, I was suddenly plunged into the role of caregiver for my then 75-year-old father, who had vascular dementia. His short-term memory was severely impaired, as were his judgment and reasoning skills. At the outset, I knew very little about dementia and next to nothing about caregiving, and fumbled my way through one challenge after another. With experience, I grew more competent and confident.
While everyone’s situation is different, and every individual unique, here are six insights that helped me help my father.
Keep in mind that many people lack a practical understanding of dementia
My stepmother never could understand, or accept, that there were things her husband could no longer do. She’d get frustrated and angry with him for forgetting things and misplacing items. When she fell gravely ill, her son was upset that my father expressed no sympathy, though my father lacked the cognitive capacity to grasp that his wife was sick. To my dismay, this misunderstanding led to a major family rift.

Even health workers can have surprisingly little understanding of dementia. A geriatric-psych nurse informed me that my father would be discharged from the hospital back to his house, where his wife could look after him – when his wife no longer lived there. The nurse had taken my father’s words at face value, though his version of reality was unreliable and out of date. For me, this was a turning point: I realised I had to become not just my father’s caregiver but his care advocate.
Set achievable goals
My father had no awareness that he had dementia and adamantly refused my attempts to help him. I hired an eldercare manager to help me figure out a way around this. When I told her I wanted to keep him safe, she said that was impossible: I could only try to keep him safer. That small grammatical shift helped me hugely: it changed my task from impossible to doable. I came to terms with the fact that I couldn’t work miracles, but I could try to make the conditions of my dad’s daily life less dangerous, less frightening, more comfortable, more enjoyable.
Communicate kindly
My dad would startle if I came up behind him and started to speak. It was better to face him and say “Dad!” to get his attention first. No long speeches, no convoluted questions; I had to speak in small, simple chunks and give him time to respond. He became very sensitive to my tone. If I sounded stern, impatient or critical, he became anxious. Speaking to him calmly helped him stay calm. I tried to give him as much choice as I could in daily, domestic matters, but choices often overwhelmed him. So I’d keep it simple: black olives or green? If he hesitated or began to fret, I’d offer to decide for him, an option he often took.
Distraction can be useful
My father was prone to abrupt mood swings; he could be lighthearted one moment and morose the next. He tended to ruminate, to get stuck in a mental groove about one of his habitual worries (like whether his taxes had been paid). I found that I could sometimes distract and reorient him if I caught it early, by introducing something amusing or fun that would catch his attention. “What’s this?” I’d ask, pointing to a nearby object. Or “How about a poem?” – because reciting poetry was his joy.
You may be shamed or judged for your caregiving choices
A taxi driver who I spoke to about my attempts to get my dad into care immediately went on a rant, saying, “Old people should be cared for by family!” I explained that my dad had nobody to help him but me and I lived overseas. The driver berated me for mistreating my dad. I realised that strangers would judge me without trying to understand my family situation. It was infinitely more painful, though, when my own father, in a state of agitation, told me that I was his only problem.
People from all walks of life need quality dementia care, and caregivers need support
In seeking out dementia care for my dad, I must have toured a dozen different care facilities. The variations were striking, and heartbreaking. How much living space the residents had, how much privacy, what activities were available, how they were spoken to, how they were treated. While some underfunded facilities provided excellent care and some well-funded facilities did not, too often money bought comfort. Dignity was on offer – for a fee. I witnessed first-hand people living (and working) in disgraceful conditions. All people living with dementia deserve quality care. And those involved in caring for someone with dementia – which currently about 1.5 million people in Australia are doing – need ongoing support, including respite.
In my case, it was essential to take breaks from my father’s company, given his endlessly repetitive conversation, as well as the emotional toll of watching his cognitive decline. Just an hour or two spent on my own or with a friend could do wonders to refresh my flagging mental state. In fact, if I had to do it all again, the one thing I would do differently is take better care of myself. I was so focused on my father’s care that I badly neglected my own.
Looking after someone whose mind no longer functions as it once did can be rewarding – my father and I shared plenty of tender moments of connection. It can also be enormously challenging – practically, emotionally, financially, legally. Addressing these challenges on a broader scale will require the political will, and a groundswell of public support, for the funding of quality dementia research, education, prevention and care.
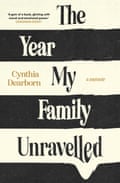
Cynthia Dearborn’s memoir The Year My Family Unravelled is out now through Affirm Press
